From Kyoto University to Startup: Innovation Rooted in Academic Excellence
To begin, could you please introduce your company?
Mr. Suzuki: HiLung Inc. is a biotechnology company founded with the mission of accelerating the development of advanced therapies for respiratory diseases, based on cutting-edge science in lung regenerative biology and tissue engineering.
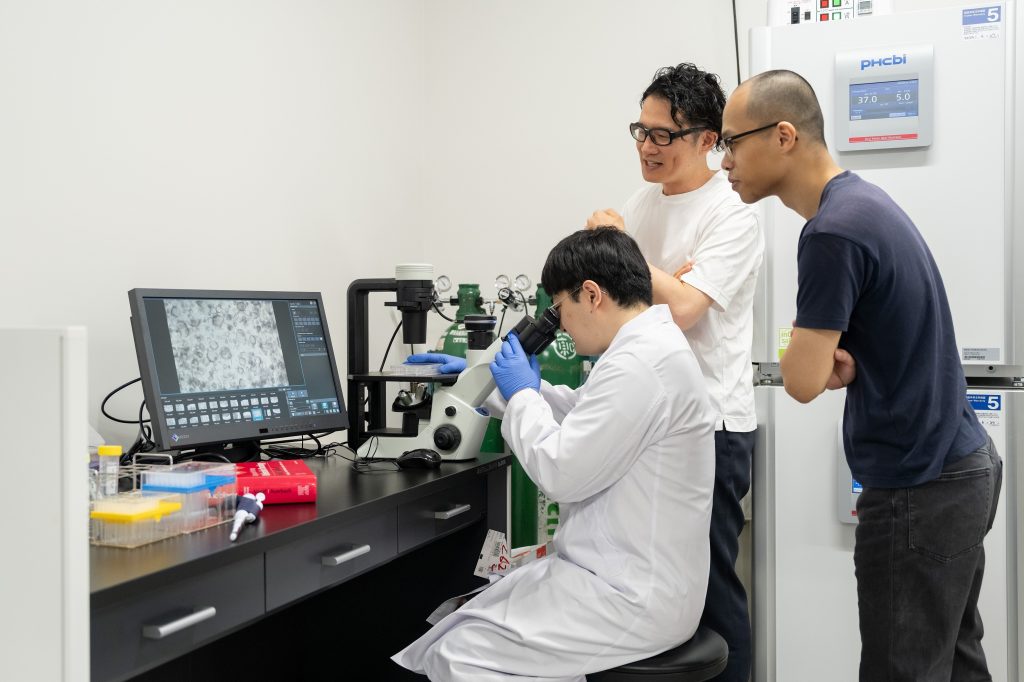
We specialize in drug discovery, toxicity testing, and regenerative research specific to the lung, and leverage proprietary technologies derived from human iPS cells to drive innovation. In addition to in-house R&D, we also offer a broad range of CRO (contract research organization) services, including support for drug development, viral infection models, and lung toxicity evaluations.
Dr. Yuki Yamamoto, our founder and CEO, achieved a major breakthrough while at Kyoto University. He successfully induced the differentiation of human alveolar epithelial cells from iPS cells, overcoming a long-standing challenge in the field. This technology serves as the foundation of our company, which was established in 2020.
Today, our operations are centered around two main locations: our headquarters in Kyoto and our translational science center in Kashiwa-no-ha. We also actively dispatch research staff to partner institutions in Japan and abroad, enabling flexible and responsive collaboration through on-site engagement.
(For more, please refer to our Nature advertisement article published on May 15, 2025.)

HiLung originated as a university-based startup, correct?
Mr. Suzuki: Yes, that's right. I would describe our current position as one that sits right between academia and industry. On the industrial side, we leverage our proprietary human iPSC-derived lung organoid technology to build disease models for respiratory conditions that have traditionally been difficult to replicate in vitro. Using these models, we provide high-resolution CRO services that assess drug efficacy and safety at both the single-cell and spatial levels.
Through this platform, we can visualize and quantify precisely where and how a drug works — and also where and why it might not work. This allows us to deliver practical, actionable feedback to pharmaceutical partners.
Drawing on my background as both a respiratory physician and a board-certified medical oncologist, I contribute not only data but also clinical insight into the strategic direction of drug development. In recent years, we’ve also seen increasing demand for our platform to evaluate lung toxicity caused by environmental toxicants and viral infections, expanding the scope of our applications significantly.
At the same time, our activities extend well beyond cell distribution and drug screening support. At its core, our research begins with a fundamental question: how can we reconstruct the human lung and decipher what is happening inside it? This motivation underpins our work across a range of fields — not only disease mechanism studies and environmental exposure research, but also regenerative medicine and aging.
Our vision at HiLung is to help unlock the human lung — one of the final frontiers in medicine — and to pave the way for the next generation of biomedical innovation and healthcare.
Could you explain what an "alveolar organoid" is?
Mr. Suzuki: An alveolar organoid is a three-dimensional structure derived from human iPS cells, designed to closely resemble human lung tissue. Culturing respiratory epithelial cells from the human lung in a stable and reproducible manner has long been considered a major challenge. However, through our proprietary differentiation protocols, we’ve succeeded in reliably generating lung epithelial cells with functions comparable to those found in vivo.
These lung organoids are used in a variety of applications — for example, to evaluate the efficacy of drug candidates before they are administered to humans, or to assess the cytotoxicity of human-infectious agents such as viruses.
Mr. Choi One of our key research areas is environmental exposure. We use our lung organoids to study how various airborne pollutants — including PM2.5, diesel exhaust particles, and tobacco smoke — affect human lung cells.
This is a critical area of research not only from the perspective of lung diseases and cancer, but also in fields like environmental policy and materials science. Human lung models offer an invaluable platform for generating scientific evidence to inform air quality regulations and ensure the safety of new materials.

Striving to Deliver the Next Breakthrough in Respiratory Disease Treatment
What are the unique features of your “alveolar organoids”?
Mr. Suzuki: In simple terms, our alveolar organoids are miniature versions of the human alveolar region, recreated in a test tube. What makes them particularly distinctive is that they’re derived from human iPS cells — meaning they are generated from the human “blueprint.” As a result, they exhibit remarkably realistic and human-specific biological responses.
Traditionally, many studies in respiratory research have relied on mouse lungs. However, the truth is that mouse and human lungs are fundamentally different. Take pulmonary fibrosis, for instance — the process where lung tissue becomes stiff and scarred. In mice, fibrosis typically develops around the bronchi and often resolves over time. In contrast, in humans, it usually starts in the peripheral regions just beneath the pleura and, once established, is irreversible.
In other words, "curable mice disease" and "human disease that does not cure" are completely different, and in drug research using such "different diseases" as models, it has become difficult to find drug candidates that work in humans. It is the history of respiratory medicine.
Our alveolar organoids help bridge this gap by faithfully replicating key features of irreversible human lung disease in vitro. That’s one of their greatest strengths.
Moreover, these organoids can be consistently produced with stable quality, enabling both high reproducibility and scalability — essential qualities for drug discovery and toxicology testing.
It seems your platform has applications across a wide range of respiratory diseases?
Mr. Suzuki: Yes, absolutely. Our technology is being applied to a broad spectrum of respiratory conditions — from major diseases like pulmonary fibrosis, COPD, and lung cancer to rare diseases such as cystic fibrosis. With alveolar organoids, we’re now able to visualize disease progression and drug responses at the cellular level, offering insight into the “entry points” and progression of diseases that were previously difficult to study.
Both Dr. Yamamoto and I come from clinical backgrounds as pulmonologists, and our co-founder Dr. Nagamoto is a pediatrician who has been deeply involved in neonatal and pediatric respiratory care. In our clinical practice, we often faced limitations — the painful reality that there are diseases we simply can’t cure. These experiences made it clear to us that a bridge was needed between bedside medicine and basic research. That realization is what led to the founding of HiLung.
Take idiopathic pulmonary fibrosis (IPF), for example. It’s a progressive, incurable condition with an unknown cause. Many patients ultimately succumb to respiratory failure or complications like infection. The average survival is just a few years, with significant individual variation, making management difficult for both patients and healthcare providers. And yet, compared to diseases like lung cancer, public awareness of IPF remains low, and research and drug development are still lagging far behind.
That’s exactly why we’ve focused on developing technologies that make the invisible visible — using miniature lungs, or organoids, to observe what's actually happening inside the human lung in real time. By capturing early disease changes and drug responses at the cellular level, we believe our platform provides a critical foundation for researchers and pharmaceutical companies to discover and develop new treatments.
Is your alveolar organoid technology also applicable to regenerative medicine?
Mr. Suzuki: Yes, we see great potential in the field of regenerative medicine as well. Of course, we're not yet at the stage where artificially generated alveolar cells can be directly transplanted into human patients. However, the foundational technologies required for such applications are steadily being developed and refined.
Our goal is not simply to create clusters of cells, but to build a living model that faithfully replicates the physiological environment, structure, and function of the human lung. Such models are already proving highly valuable for drug discovery and toxicity testing, and in the future, they may serve as a stepping stone toward cell-based regenerative therapies and even organ reconstruction.
What are your "strengths"?
Mr. Suzuki: As far as I know, we are the only one in the world that has the technology to stably cultivate alveoli epithelial cells derived from human iPS cells. In addition, our unique strength is the technology to produce miniature organs = alveoli organoids built using these cells.
There are companies that provide airway epithelial cells derived from human lungs overseas, but since they mainly use primary cells (cells taken directly from living organisms), there are issues in the variability of each cell and the quantity and stability of supply.
In this regard, our technology is capable of providing highly reliable research models in fields such as drug discovery and toxicity evaluation by combining quality stability and reproducibility with mass production by guiding the target cell type from human iPS cells.
In addition, although we have a small team, each and every member of the international community has a proven track record in each field. As a group of experienced people across the clinical, academic, and pharmaceutical industries, the development of research and services is based on natural and global cooperation. Currently, we have approximately the same number of international contracts as domestic contracts.
From Kashiwa-no-ha to the World:Pioneering Global Collaborations in Cutting-Edge Biomedical Science
What led you to establish your presence at "Mitsui Link Lab Kashiwa-no-ha 1"?
Mr. Suzuki: We chose Kashiwa-no-ha because we felt it offered a unique environment where cutting-edge academic research and industrial innovation could intersect. Even before joining HiLung, I had strong ties to this area — I had been collaborating with Professor Yutaka Suzuki at the University of Tokyo as part of an AMED drug discovery platform project, and as a clinician, I had also worked with Dr. Katsuya Tsuchihara at the National Cancer Center Hospital East through cancer genome expert panel activities.
These connections laid the groundwork for deeper engagement in the region. Around the time our CEO, Dr. Yamamoto, published our core technology in Nature Methods, our collaborative research with Professor Yutaka Suzuki began to accelerate. Being exposed to the rapidly evolving world of omics and spatial biology further strengthened my conviction that we needed to establish a base here in Kashiwa-no-ha. It felt like a natural next step — one that would allow us to push the boundaries of innovation through close collaboration with some of the world’s leading institutions.

It’s been almost a year since you moved in. How do you feel about the environment here?
Mr. Suzuki: I feel it’s a truly great environment. When I hit a creative block, I often head down to the café on the first floor — it’s a great place to grab a coffee and casually chat with staff from other companies. I really appreciate those moments.
During lunchtime, you’ll sometimes find researchers and staff from the neighboring National Cancer Center Hospital East, which naturally creates opportunities to connect with people from diverse backgrounds.
Occasionally, the conversations have nothing to do with research or development — just everyday small talk — but even those light-hearted exchanges can spark unexpected insights or new ideas. In the end, they often come full circle and enrich our work.
It’s more than just a lab — it’s a place where people and knowledge intersect, and that’s what makes it so special.
Do you have any opportunities to interact with other residents of Kashiwa-no-ha Lab?
Mr. Suzuki: Yes, in fact, the pharmaceutical companies that are taking care of their work also live in the same Kashiwa-no-ha laboratory, and when you meet in the corridor, you may feel free to exchange information about trends in cutting-edge technologies. In addition, lunchtime tips and other events are held regularly, and we are actively participating in this event. I feel that it is a very thankful environment in that such a place of exchange is naturally born.
Finally, please tell us about your future prospects.
Mr. Suzuki: At present, we are steadily expanding both domestically and internationally in areas such as our organoid-based drug discovery CRO services and our analytical services utilizing virus infection models. These business lines are gaining traction and entering a stable growth phase.
Looking ahead, our next major challenge is to bring to society a novel evaluation model capable of predicting and detecting unknown pulmonary toxicity risks. Leveraging our prime location adjacent to the National Cancer Center Hospital East, we hope to work closely with partner institutions to propose organoid-based platforms that can preemptively assess drug-induced lung toxicity, particularly from anticancer agents. Ultimately, we aim to establish a system that can provide actionable feedback—such as identifying which molecular modifications may reduce pulmonary toxicity—and share this innovation globally. In addition, for the MPS (Microphysiological Systems) models currently under development, we are working toward implementing a platform that enables the visualization and quantification of respiratory functions, such as lung capacity, as novel indicators of drug efficacy.
One pioneering example is HL001, a candidate therapy for pulmonary fibrosis co-developed under the support of AMED. Based on efficacy data sensitively detected using our lung organoid models, this compound was granted orphan drug designation by the U.S. FDA. We believe it represents a promising new treatment option for intractable diseases.